contact
Shereece Singleton
Office Manager
F 410-706-0865
Diagnostics for biofilm infections
 Biofilms are notoriously difficult to diagnose since the small nidus of infection is often missed when tissue is extracted for culture. It is important to discern whether the infection is a localized biofilm or a free floating planktonic infection since the treatment modalities for these two forms of infections are significantly different. In particular, biofilm infections, in converse to the planktonic modes of infection, are resistant to clearance by antimicrobial agents.
Biofilms are notoriously difficult to diagnose since the small nidus of infection is often missed when tissue is extracted for culture. It is important to discern whether the infection is a localized biofilm or a free floating planktonic infection since the treatment modalities for these two forms of infections are significantly different. In particular, biofilm infections, in converse to the planktonic modes of infection, are resistant to clearance by antimicrobial agents.
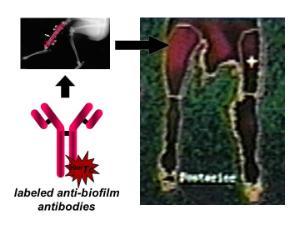
In order to better diagnose biofilm infections, we have developed a rapid biofilm lateral flow immunoassay that detects host antibodies generated against biofilm specific proteins in the sera as well as an in vivo diagnostic agent that is based upon labelled antibodies against biofilm specific antigens that can be injected into the host and localize at areas of biofilm infection.
Broad, Long-term Objectives
Staphylococcus aureus is a Gram-positive, pathogenic bacterial species responsible for greater than 340,000 instances of infection that end in hospitalization, and nearly 60,000 annual deaths, in the United States. One of the most important mechanisms that S. aureus uses to persist within the host—particularly in the case of orthopedic infection—is through a biofilm mode of growth. S. aureus is recalcitrant to host immunity and antimicrobials after it forms a mature biofilm. Because of the physical presence of the biofilm community on native tissue or abiotic implants, the nidus of infection must usually be removed in order to resolve the infection. Diagnosis of the biofilm infection while the biofilm was still in an immature state would allow for earlier inception of antibiotic treatment and clearance of the organism, resulting in fewer invasive procedures. Even in cases where the biofilm has matured to a resistant state, the accurate diagnosis of a biofilm infection is still important to guide treatment and rule out a diagnosis of aseptic loosening of an indwelling medical device as well as determining whether or not infection has been cleared prior to re-implantation following device removal. An important property of biofilm is its distinctive phenotype compared to taxonomically identical microorganisms grown in planktonic (suspended cell) culture. The determination of protein antigens specific to biofilms and expressed on the bacterial cell surface would allow for approaches that take advantage of this unique expression pattern to diagnose a biofilm infection. Therefore, our long term objective is to utilize proteomics and the host antibody response to characterize S. aureus biofilms in molecular detail so as to identify protein antigens that are both biofilm-specific, located on the cell-surface and immunogenic during infection. Recombinant versions of these selected proteins will be produced and purified. These purified antigens will then be affixed to a surface in a lateral flow immunoassay and then probed with sera from infected patients suffering from S. aureus biofilm infections. The host antibodies against these specific biofilm antigens in the sera samples will then be detected. Another diagnostic system will also be developed using these recombinant biofilm antigens in which polyclonal antibodies will be made against them in a rabbit. These anti-biofilm antibodies will then be conjugated to detectable markers, injected into the host to localize S. aureus biofilm infection in vivo by two animal models.
Rationale/Challenge of an Existing Paradigm
Current means of diagnosis of biofilm-mediated orthopedic infection are lacking. Imaging methods, including radiography, CT scan, MRI, and radionuclide scans all feature low sensitivities and specificities, leading to false diagnoses of sterile inflammation when infection is present or vice versa. While biopsy and culture remains the gold standard of diagnosis, contamination of the biopsy or sampling from a draining sinus tract (instead of directly from the bone), can lead to aberrant results. In addition, culturing all to often results in false negative results because the culture sample is often obtained from an area close but not at the localized biofilm nidus of infection. Therefore, diagnostic tools that can determine whether or not the patient is suffering from a S. aureus biofilm infection as well as one that localizes at the infection location would provide increased sensitivity and specificity while also decreasing the need for biopsy and culture. This would lead to an earlier inception of the proper antibiotic treatment, less need for surgical intervention, identifying infections in cases of supposed aseptic loosening, and result in an overall lessening of patient morbidity, mortality and cost of care.
Goal of the Srecific Research Proposed
To conduct the studies enumerated in the specific aims to prove the validity of the following hypothesis.
Hypothesis
We hypothesize that the phenotypic distinctiveness of S. aureus biofilm cells will allow for the identification of biofilm-specific antigens that can be used as markers for the accurate diagnosis of S. aureus biofilm infections.
Specific Aims
-
Identify S. aureus proteins that are both expressed and immunogenic during biofilm-associated orthopaedic infection in an animal model.
-
Demonstrate the efficacy of the lateral flow immunoassay to detect host anti-biofilm antibodies against S. aureus biofilm-specific antigens and diagnose S. aureus biofilm infections in two animal models and human hosts.
-
Demonstrate the in vivo diagnostic efficacy of immunovisualization using antibodies generated against the S. aureus biofilm-specific antigens in animal models of implant infection and chronic osteomyelitis.